Notes
COMMON TYPES OF INTRAVENOUS (IV) FLUIDS AND THEIR USES

Intravenous fluids are additional fluids used in intravenous therapy to restore or maintain normal fluid volume and electrolyte balance in situations where oral route is not possible, or fluid volume needs to be restored immediately.
TYPES OF INTRAVENOUS FLUIDS
Intravenous fluids can be categorized into two main types namely, Crystalloids and Colloids.
CRYSTALLOIDS: these are solutions that contain small molecules that flow easily across semipermeable membranes, from the bloodstream into the cells and body tissues. Crystalloid solutions are distinguished by the relative tonicity (before infusion) in relation to plasma and are categorized as isotonic, hypotonic, or hypertonic.
Isotonic IV Fluids: Isotonic solutions have a concentration of dissolved particles like plasma, and an osmolality of 250 to 375 mOsm/L. These fluids remain within the extracellular compartment and are distributed between intravascular (blood vessels) and interstitial (tissue) spaces, increasing intravascular volume. They are used primarily to treat fluid volume deficit. Examples of isotonic iv fluids include: 0.9% NaCl (Normal Saline), Ringer’s Lactate (LR).
Hypotonic IV Fluids: Hypotonic solutions have a concentration of dissolved particles lower compared to plasma and an osmolality < 250 mOsm/L. Hypotonic fluids lower serum osmolality within the vascular space by causing fluid to shift out of the blood into the cells and tissue spaces. Typically used to treat conditions causing intracellular dehydration, such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. Examples of hypotonic iv fluids include ½ (0.45%) Normal Saline (1/2 Ns)
Hypertonic IV Fluids: Hypertonic solutions have a concentration of dissolved particles higher than plasma and an osmolality > 375 mOsm/L. A higher solute concentration causes the osmotic pressure gradient to draw water out of cells, increasing extracellular volume. These fluids are often used as volume expanders and may be prescribed for hyponatremia (low sodium). They may also benefit patients with cerebral edema. Examples of hypertonic iv fluids include Dextrose 5% in 0.45% NaCl, Dextrose 50% in Water (D50W), Dextrose 5% in 0.9% NaCl (D5NS).
NORMAL SALINE (NS)
DESCRIPTION
- 0.9% NaCl in Water
- Crystalloid Solution
- Isotonic (308 mOsm)
USES
- Increases circulating plasma volume when red cells are adequate.
- Shock
- Fluid replacement in patients with diabetic ketoacidosis
- Hyponatremia
- Blood transfusions
- Resuscitation
- Metabolic alkalosis
- Hypercalcemia
- Replaces losses without altering fluid concentrations.
PRECAUTIONS
- Do not use in patients with heart failure, edema, or hypernatremia, because NS replaces extracellular fluid and can lead to fluid overload.
1/2 NORMAL SALINE (1/2 NS)
DESCRIPTION
- 0.45% NaCl in Water
- Crystalloid Solution
- Hypotonic (154 mOsm)
USES
- Water replacement
- Raises total fluid volume.
- DKA after initial normal saline solution and before dextrose infusion
- Hypertonic dehydration
- Sodium and chloride depletion
- Gastric fluid loss from nasogastric suctioning or vomiting.
- Useful for daily maintenance of body fluid but is of less value for replacement of NaCl deficit.
- Helpful for establishing renal function.
PRECAUTIONS
- Use cautiously; may cause cardiovascular collapse or increase in intracranial pressure.
- Don’t use in patients with liver disease, trauma, or burns
LACTATED RINGER’S (LR) OR RINGER’S LACTATE (RL)
DESCRIPTION
- Normal saline with electrolytes and buffer
- Isotonic (275 mOsm)
USES
- Replaces fluid and buffers pH.
- Hypovolemia due to thirdspace shifting.
- Dehydration
- Burns
- Lower GI tract fluid loss
- Acute blood loss
PRECAUTIONS
- Don’t use in liver disease because the patient can’t metabolize lactate; a functional liver converts it to bicarbonate; don’t give if patient’s pH > 7.5.
- Has potassium therefore don’t use to patients with renal failure as it can cause hyperkalemia.
D5W (5%DEXTROSE WATER) OR 5% DEXTROSE
DESCRIPTION
- Dextrose 5% in water Crystalloid solution
- Isotonic (in the bag)
- *Physiologically hypotonic (260 mOsm) (the dextrose is metabolized quickly so that only water remains – a hypotonic fluid).
USES
- Raises total fluid volume.
- Helpful in rehydrating and excretory purposes.
- Fluid loss and dehydration
- Hypernatremia
- Provides 170-200 calories/1,000cc for energy.
PRECAUTIONS
- Use in caution to patients with renal or cardiac disease, can cause fluid overload.
D5NS
DESCRIPTION
- Dextrose 5% in 0.9% saline
- Hypertonic (560 mOsm)
USES
- Hypotonic dehydration
- Replaces fluid sodium, chloride, and calories.
- Temporary treatment of circulatory insufficiency and shock if plasma expanders aren’t available.
- SIADH (or use 3% sodium chloride).
- Addisonian crisis
PRECAUTIONS
- Do not use in patients with cardiac or renal failure because of danger of heart failure and pulmonary edema.
- Watch for fluid volume overload.
D5 1/2 NS
DESCRIPTION
- Dextrose 5% in 0.45% saline
- Hypertonic (406 mOsm)
USES
- DKA after initial treatment with normal saline solution and half-normal saline solution – prevents hypoglycemia and cerebral edema.
- Most common postoperative fluid
- Useful for daily maintenance of body fluids and nutrition, and for rehydration.
PRECAUTIONS
In DKA, use only when glucose falls < 250 mg/dl.
D5LR
DESCRIPTION
- Dextrose 5% in Lactated Ringer’s
- Hypertonic (575 mOsm)
USES
- Same as LR plus provides about 180 calories per 1000cc’s.
- Indicated as a source of water, electrolytes, and calories or as an alkalinizing agent.
PRECAUTIONS
- Contraindicated in newborns (≤ 28 days of age), even if separate infusion lines are used (risk of fatal ceftriaxone-calcium salt precipitation in the neonate’s bloodstream).
- Contraindicated in patients with a known hypersensitivity to sodium lactate.
NORMOSOL-R
DESCRIPTION
- Normosol
- Isotonic (295 mOsm)
USES
- Replaces fluid and buffers pH.
- Indicated for replacement of acute extracellular fluid volume losses in surgery, trauma, burns or shock.
- Used as an adjunct to restore a decrease in circulatory volume in patients with moderate blood loss.
PRECAUTIONS
- Not intended to supplant transfusion of whole blood or packed red cells in the presence of uncontrolled hemorrhage or severe reductions of red cell volume.
COLLOIDS
These are solutions that contains large molecules that do not pass through semipermeable membranes and therefore remain in the blood vessels. Also known as volume/plasma expanders, colloids expand intravascular volume by drawing fluid from the interstitial space into the vessels through higher oncotic pressure. Less total volume is required compared to IV fluids. Colloids are indicated for patients in malnourished states and patients who cannot tolerate large infusions of fluid. Examples of colloids are Albumin (5%), Albumin (25%) and Hetastarch (6%).
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Notes
Understanding Hypotension: Types, Causes, and Symptoms
Hypotension, commonly referred to as “low blood pressure,” is a medical condition in which the blood pressure in the arteries is lower than normal (when the blood pressure reading is lower than 90/60mmHg). There are various types of hypotension, each with different causes, symptoms, and treatments. As a nurse, it is important to be aware of the different types of hypotension and their management in order to provide safe and effective care to your patients.
Orthostatic hypotension
Orthostatic hypotension is a type of hypotension that occurs when a person changes position from lying down or sitting to standing up. This can cause a sudden drop in blood pressure, leading to symptoms such as dizziness, lightheadedness, and fainting. Orthostatic hypotension is common in older adults, especially those with underlying medical conditions such as Parkinson’s disease, diabetes, or autonomic neuropathy.
The management of orthostatic hypotension involves lifestyle modifications, such as avoiding sudden changes in position, staying hydrated, and wearing compression stockings. Medications such as fludrocortisone, midodrine, and droxidopa may also be prescribed to help raise blood pressure.
Neurally mediated hypotension.
Neurally mediated hypotension also known as the fainting reflex, neurocardiogenic syncope, vasodepressor syncope, the vaso-vagal reflex, and autonomic dysfunction is a type of hypotension that occurs in response to certain triggers, such as standing for a long time or exposure to heat. It is caused by a malfunction of the autonomic nervous system, which regulates blood pressure and heart rate. Neurally mediated hypotension can cause symptoms such as dizziness, nausea, and fainting. Other symptoms may include confusion, muscle aches, headaches, and chronic fatigue.
The treatment of neurally mediated hypotension involves avoiding triggers and increasing fluid and salt intake.
Severe hypotension
Severe hypotension is a medical emergency that requires immediate treatment. It is characterized by a sudden and severe drop in blood pressure, which can lead to organ damage and even death if not promptly addressed. Severe hypotension can be caused by various conditions, such as sepsis, anaphylaxis, or a heart attack.
The management of severe hypotension involves identifying and treating the underlying cause. This may involve administering intravenous fluids, medications such as vasopressors or inotropes, and oxygen therapy. In severe cases, mechanical ventilation or extracorporeal membrane oxygenation (ECMO) may be necessary.
Postprandial hypotension
It is common in older adults and those with underlying medical conditions such as diabetes, Parkinson’s disease, or autonomic neuropathy. Postprandial hypotension is a type of hypotension that occurs after eating a meal. After eating, the heart rate ramps up to send blood flowing to the digestive system, but with this type of low blood pressure, the mechanism fails, resulting in dizziness, lightheadedness, and fainting.
The management of postprandial hypotension involves eating smaller, more frequent meals and avoiding large meals high in carbohydrates or fats. Medications such as acarbose, midodrine, and caffeine may also be prescribed.
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Notes
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE), A COMMONLY MISDIAGNOSED MEDICAL CONDITION

Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease that can affect various organ systems in the body. It is characterized by the production of autoantibodies against self-antigens, leading to chronic inflammation and tissue damage including the joints, skin, kidneys, blood cells, brain, heart, and lungs. SLE is a heterogeneous disease with a wide range of clinical manifestations, making it difficult to diagnose and manage.
PATHOPHYSIOLOGY
The pathophysiology of SLE involves a complex interplay between genetic, environmental, hormonal, and immunologic factors. Multiple genetic loci have been associated with SLE, including genes involved in immune system function and regulation. Environmental factors such as infections, medications, and ultraviolet light exposure have also been implicated in the development of SLE.
In SLE, immune dysregulation leads to the production of autoantibodies against nuclear components such as DNA, RNA, and histones. These autoantibodies form immune complexes that deposit in various tissues, leading to chronic inflammation and tissue damage. Additionally, immune dysregulation can lead to aberrant T-cell activation, cytokine production, and complement activation, further contributing to the pathogenesis of SLE.
CAUSES
The exact causes of SLE are not fully understood, but a combination of genetic, environmental, hormonal, and immunologic factors are thought to contribute to its development. Women are more commonly affected than men, and the disease often presents during the childbearing years. Genetic factors are estimated to account for up to 66% of the risk for developing SLE. Environmental factors such as infections, medications, and ultraviolet light exposure have also been implicated in the development of SLE.
CLINICAL MANIFESTATIONS
The clinical manifestations of SLE are diverse and can affect multiple organ systems in the body. Common symptoms include fatigue, fever, joint pain and swelling, skin rashes, and photosensitivity. SLE can also cause more serious complications such as lupus nephritis, which is a major cause of morbidity and mortality in patients with SLE.
ASSESSMENT AND DIAGNOSTIC FINDINGS
The diagnosis of SLE is based on a combination of clinical and laboratory findings. The American College of Rheumatology has developed diagnostic criteria for SLE, which require the presence of at least four of the following: malar rash, discoid rash, photosensitivity, oral ulcers, arthritis, serositis, renal disorder, neurologic disorder, hematologic disorder, immunologic disorder, and antinuclear antibody positivity. Laboratory tests that may be helpful in diagnosing SLE include antinuclear antibody (ANA) testing, anti-double-stranded DNA (anti-dsDNA) antibody testing, and complement-level testing.
MEDICAL MANAGEMENT
The management of SLE involves a multidisciplinary approach, including rheumatologists, nephrologists, dermatologists, and other specialists as needed. Treatment goals include controlling disease activity, preventing flares, and minimizing organ damage. Treatment options may include nonsteroidal anti-inflammatory drugs (NSAIDs), antimalarial drugs, glucocorticoids, immunosuppressants, and biological agents.
PHARMACOLOGIC MANAGEMENT
Pharmacologic management of SLE involves a range of medications targeting different aspects of the disease’s pathophysiology. NSAIDs can be used to manage mild to moderate pain and inflammation, while antimalarial drugs such as hydroxychloroquine can be used to prevent disease flares and reduce disease activity. Glucocorticoids such as prednisone can be used to manage severe disease activity and organ involvement, but their long-term use is associated with significant adverse effects. Immunosuppressive agents such as azathioprine, mycophenolate mofetil, and cyclophosphamide can be used to control disease activity and prevent organ damage. Biologic agents such as belimumab, a monoclonal antibody targeting B-cell activating factor, have also been approved for the treatment of SLE.
Systemic lupus erythematosus diagnosis and management, https://academic.oup.com/rheumatology/article/56/suppl_1/i3/2738661.
C. (2023, January 31). Systemic lupuserythematosus (SLE). Centers for Disease Control and Prevention. https://www.cdc.gov/lupus/facts/detailed.html
Systemic lupus erythematosus pathophysiology – wikidoc. (n.d.). Systemic Lupus Erythematosus Pathophysiology – Wikidoc. https://www.wikidoc.org/index.php/Systemic_lupus_erythematosus_pathophysiology
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Notes
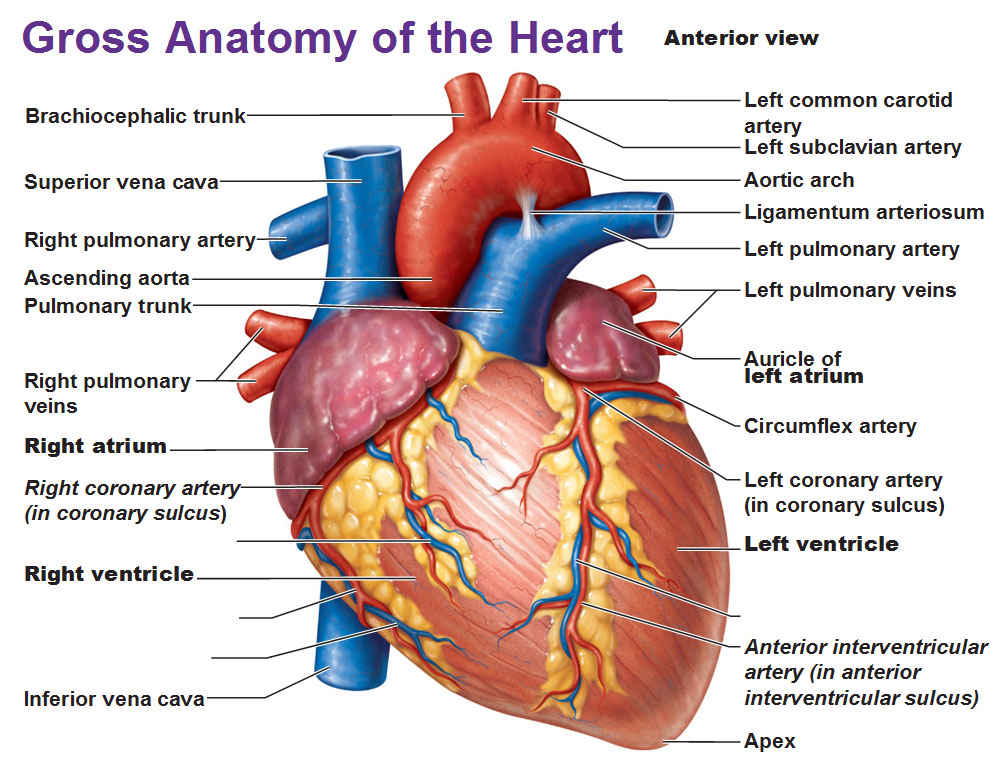
TYPES OF SHOCK
Shock is a threatening life condition of circulatory failure which causes inadequate oxygen delivery to meet cellular metabolic needs and oxygen consumption requirements, producing cellular and tissue hypoxia. The effects of shock are initially reversible, but rapidly become irreversible, resulting in multiorgan failure (MOF) and death. When a patient presents with undifferentiated shock, it is important that the clinician immediately initiate therapy while rapidly identifying the etiology so that definitive therapy can be administered to reverse shock and prevent MOF and death.
There are four main types of shock:
1. Anaphylactic shock
2. Cardiogenic shock
3. Hypovolemic shock
4. Septic shock
Anaphylactic shock is a severe and sudden allergic reaction that can occur after exposure to an allergen. Symptoms include swelling of the face and throat, difficulty breathing, and a drop in blood pressure. Anaphylactic shock can be life-threatening and requires immediate medical treatment.
Cardiogenic shock occurs when the heart is unable to pump enough blood to meet the body’s needs. This can be due to a heart attack, heart failure, or other heart conditions. Symptoms include shortness of breath, chest pain, and a weak and irregular heartbeat. Cardiogenic shock is a medical emergency and requires treatment in a hospital.
Hypovolemic shock occurs when there is a decrease in the amount of blood or fluid in the body. This can be due to blood loss from an injury, severe dehydration, or excessive vomiting or diarrhea. Symptoms include lightheadedness, fainting, and a decrease in urine output. Hypovolemic shock can be life-threatening and requires immediate medical treatment.
Septic shock. This type of shock is caused by an infection or sepsis. Sepsis is a potentially life-threatening condition that occurs when an infection spreads throughout the body. Symptoms include low blood pressure, rapid heart rate, chills, and fever. Septic shock is a medical emergency and requires treatment in a hospital.
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
-

 Nursing News5 years ago
Nursing News5 years agoLIST OF ACCREDITED GOVERNMENT NURSING AND MIDWIFERY TRAINING SCHOOLS IN GHANA
-

 Nursing News3 years ago
Nursing News3 years agoNURSING ADMISSION FORMS ON SALE FOR THE 2023/2024 ACADEMIC YEAR
-

 Nursing Procedures and Skills5 years ago
Nursing Procedures and Skills5 years agoTHE NURSES PLEDGE AND THE MIDWIVE’S PRAYER
-

 Nursing Procedures and Skills5 years ago
Nursing Procedures and Skills5 years agoNURSING TRAINING ADMISSION INTERVIEW QUESTIONS
-

 Nursing News4 years ago
Nursing News4 years agoGHS INTRODUCES TWO NEW BELT COLOURS FOR TWO NEW LEVELS IN THE NURSING AND MIDWIFERY SERVICE
-

 Nursing News4 years ago
Nursing News4 years agoMOH SUSPENDS THE 2021/2022 ACADEMIC CALENDAR FOR NURSING AND MIDWIFERY SCHOOLS
-

 Nursing News5 years ago
Nursing News5 years agoLIST OF PRIVATE NURSING AND MIDWIFERY TRAINING SCHOOLS (ACCREDITED)
-

 Nursing News4 years ago
Nursing News4 years agoGHANA COLLEGE OF NURSES AND MIDWIVES’ PROGRAMMES AND ADMISSION REQUIREMENT