Mental Health
Defense Mechanism
A defense mechanism is a coping technique that reduces anxiety arising from unacceptable or potentially harmful stimuli. Defence mechanisms are unconscious and are not to be confused with conscious coping strategies. Sigmund Freud was one of the first proponents of this construct. Here is the list of some defence mechanisms:
Compensation
Over-achievement in one area to offset real or perceived deficiencies in another area
Conversion
Expression of an emotional conflict through the development of a physical symptom, usually sensorimotor in nature
Denial
Failure to acknowledge an unbearable condition; failure to admit the reality of a situation or how one enables the problem to continue
Displacement
Ventilation of intense feelings toward persons less threatening than the one who aroused those feelings
Dissociation
Dealing with emotional conflict by a temporary alteration in consciousness or identity
Fixation
Immobilization of a portion of the personality resulting from unsuccessful completion of tasks in a developmental stage
Identification
Modelling actions and opinions of influential others while searching for identity, or aspiring to reach a personal, social, or occupational goal
Intellectualization
Separation of the emotions of a painful event or situation from the facts involved; acknowledging the facts but not the emotions
Introjection
Accepting another person’s attitudes, beliefs, and values as one’s own
Projection
Unconscious blaming of unacceptable inclinations or thoughts on an external object
Rationalization
Excusing own behaviour to avoid guilt, responsibility, conflict, anxiety, or loss of self-respect
Reaction Formation
Acting the opposite of what one thinks or feels
Regression
Moving back to a previous developmental stage to feel safe or have needs met
Repression
Excluding emotionally painful or anxiety-provoking thoughts and feelings from conscious
awareness
Resistance
Overt or covert antagonism toward remembering or processing anxiety-producing information
Sublimation
Substituting a socially acceptable activity for an impulse that is unacceptable
Substitution
Replacing the desired gratification with one that is more readily available
Suppression
Conscious exclusion of unacceptable thoughts and feelings from conscious awareness
Undoing
Exhibiting acceptable behaviour to make up for or negate unacceptable behaviour
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Mental Health
ANORGASMIA: FEMALE ORGASM DISORDER
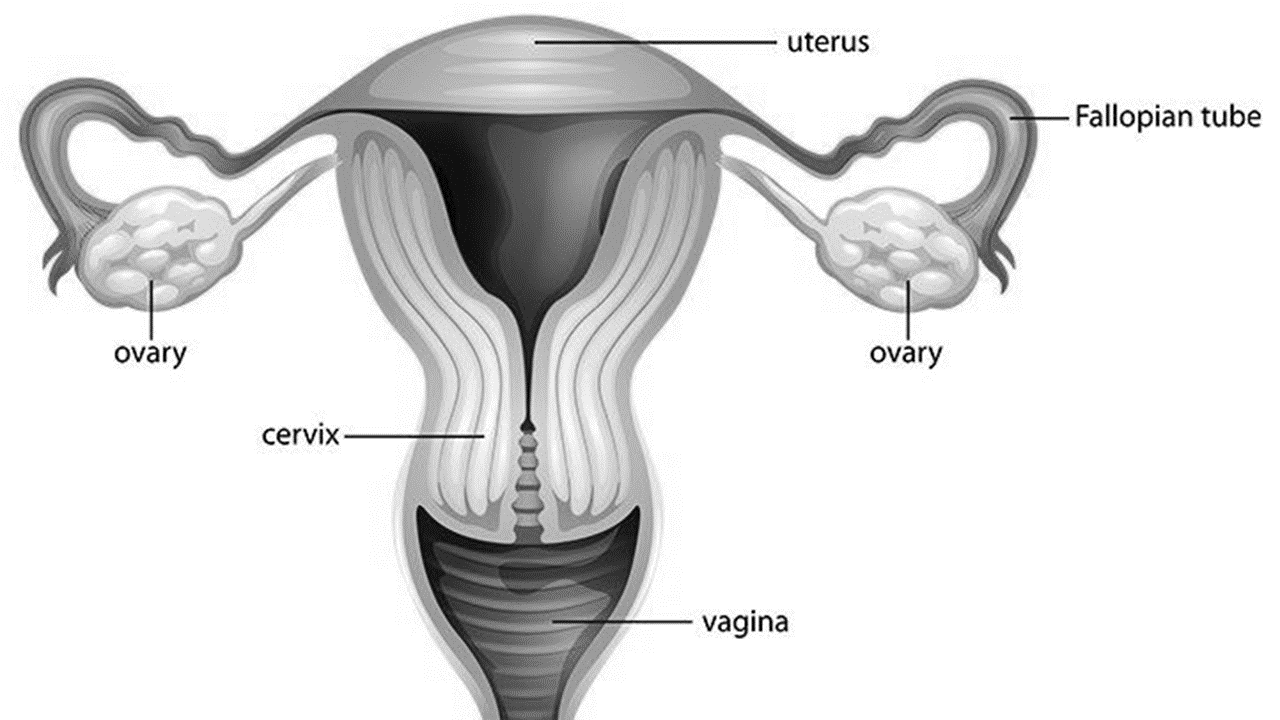
Female orgasmic disorder is a sexual dysfunctional disorder characterized by a marked delay in, marked infrequency of, or absence of orgasm as well as markedly reduced intensity of orgasmic sensations. This means that the female has a significant delay, infrequent, and absence of orgasm, and reduced intensity of orgasmic sensations. The symptoms of which should have persisted for at least six (6) months and caused clinically significant distress in the individual.
It is reported that about 10% to 42% of females have orgasmic problems depending on multiple factors such as age, culture, duration, and severity of symptoms. Approximately 10% of women do not experience orgasm throughout their lifetime. Female orgasmic disorder can be lifelong or acquired. A lifelong female orgasmic disorder indicates that the orgasmic difficulties have always been present, whereas the acquired subtype would be assigned if the woman’s orgasmic difficulties developed after a period of normal orgasmic functioning.
CAUSES/RISK FACTORS
Female orgasmic disorder has no single cause several factors may contribute to the disorder
- Psychological factors, such as anxiety and concerns about pregnancy, can potentially interfere with a woman’s ability to experience orgasm.
- Relationship problems
- Physical health problems such as diabetes, multiple sclerosis, pelvic nerve damage from radical hysterectomy, and spinal cord injury.
- Women with vulvovaginal atrophy (characterized by symptoms such as vaginal dryness, itching, and pain) are significantly more likely to report orgasm difficulties than are women without this condition
- mental health conditions, such as depression or anxiety
- Sociocultural factors (e.g. gender role expectations, sexual experience, and religious beliefs)
- History of sexual abuse
- Poor body image
TREATMENT
- The treatment basically depends on the cause.
- Increase clitoral stimulation during sexual intercourse
- Treatment of any underlying medical conditions
- Cognitive Behavioral Therapy (CBT) or Sex Therapy
- Couples Therapy: the couple has the opportunity to strengthen their communication skills, listening, emotional expression, and resolve any conflict that may influence the disorder.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Laan, E., Rellini, A.H.& Barnes, T. (2013). Standard operating procedures for female orgasmic disorder: Consensus of the International Society for Sexual Medicine. The Journal of Sexual Medicine. 10(1):74-82
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Mental Health
PSYCHIATRIC TERMINOLOGIES TO BE TRANSLATED INTO AKAN(TWI)

Terminologies in the general medical practice have often seen moderate improvement over the years with respect to translation into the various local languages. This has helped in the effective communication between health professionals and clients/patients. For nurses especially those who often communicate with the patient, this is very vital in situations where patients do not understand the English language.
Unlike in general medical practice, the issue in psychiatry is different. A lot of terminologies in psychiatry have not been translated into our local languages, especially Akan. This has been one of the major setbacks in the field of psychiatry in Ghana. As a result of this, communicating diagnosis, history taking becomes challenging sometimes. For psychiatric nurses that do health education, it becomes a major issue communicating psychiatric terminologies in our local languages to our clients and the public.
In light of this, the Mental Health Authority (MHA) together with other stakeholders is embarking on a translation of mental health terminologies into Akan (Twi) to help in effective communication between health professionals and clients/public. This started in 2018 with various mental health and language experts to translate mental health terminologies into Twi.
On 22nd December 2020, the MHA had a stakeholder meeting to validate the work done so far with representatives from the Ghana Psychological Council, Ghana Psychological Association, Ghana Prison’s Service, NGO’s in mental health, Ankaful Psychiatric Hospital, Accra Psychiatric Hospital, and Pantang Psychiatric Hospital, Ghana Health Service, Health Facilities Regulatory Agency (HeFRA), Media Houses.
According to the MHA a date for a second stakeholders meeting will be communicated soon.
SOURCE: MHA
Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
Mental Health
COVID-19, THE FATE OF PERSONS LIVING WITH MENTAL ILLNESS AND THE PSYCHIATRIC FRONTLINE HEALTH WORKERS

Discover more from Nursing In Ghana
Subscribe to get the latest posts sent to your email.
-

 Nursing News5 years ago
Nursing News5 years agoLIST OF ACCREDITED GOVERNMENT NURSING AND MIDWIFERY TRAINING SCHOOLS IN GHANA
-

 Nursing News3 years ago
Nursing News3 years agoNURSING ADMISSION FORMS ON SALE FOR THE 2023/2024 ACADEMIC YEAR
-

 Nursing Procedures and Skills5 years ago
Nursing Procedures and Skills5 years agoTHE NURSES PLEDGE AND THE MIDWIVE’S PRAYER
-

 Nursing Procedures and Skills5 years ago
Nursing Procedures and Skills5 years agoNURSING TRAINING ADMISSION INTERVIEW QUESTIONS
-

 Nursing News4 years ago
Nursing News4 years agoGHS INTRODUCES TWO NEW BELT COLOURS FOR TWO NEW LEVELS IN THE NURSING AND MIDWIFERY SERVICE
-

 Nursing News4 years ago
Nursing News4 years agoMOH SUSPENDS THE 2021/2022 ACADEMIC CALENDAR FOR NURSING AND MIDWIFERY SCHOOLS
-

 Notes5 years ago
Notes5 years agoCOMMON TYPES OF INTRAVENOUS (IV) FLUIDS AND THEIR USES
-

 Nursing News5 years ago
Nursing News5 years agoLIST OF PRIVATE NURSING AND MIDWIFERY TRAINING SCHOOLS (ACCREDITED)